Acupuncture Knee Arthritis Pain Relief Confirmed
Researchers find acupuncture effective for the treatment of knee osteoarthritis pain and joint dysfunction. Three independent studies confirm the benefits of acupuncture. One study finds acupuncture effective for increasing the efficacy of celecoxib treatment. Another finds acupuncture effective for increasing the positive patient outcome rates for patients taking Traditional Chinese Medicine (TCM) herbs. A third study compared two different types of acupuncture and determined that centro-square needling is exceptionally beneficial for the treatment of knee osteoarthritis. Let’s start with a brief overview of knee osteoarthritis and acupuncture before reviewing the independent investigations.
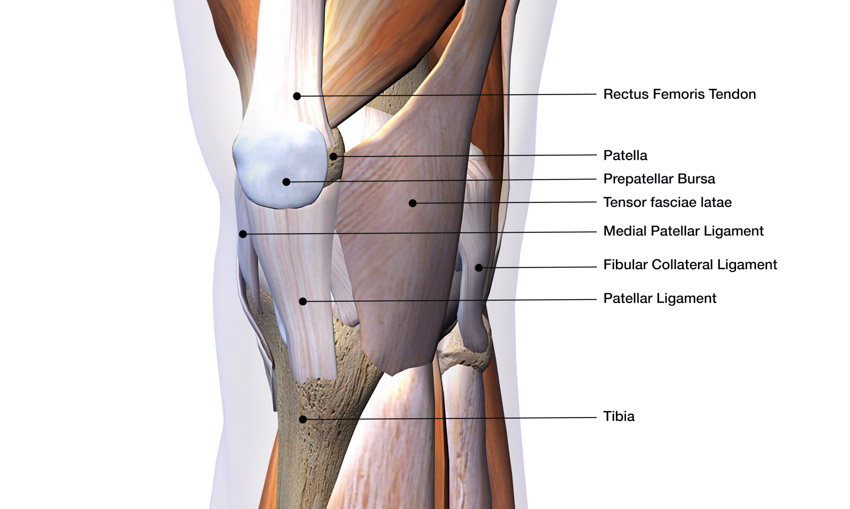
Knee osteoarthritis (KOA) is a common degenerative joint disease. It often develops from knee joint cartilage degeneration and bone hyperplasia, causing pain and limited joint movement. Long-term use of anti-inflammatory and analgesic oral medications, or intra-articular sodium hyaluronate, may lead to liver and kidney toxicity, as well as gastrointestinal damage. [1–2] It is therefore worthwhile to explore treatment methods to prevent these adverse effects.
The pathogenesis of KOA in TCM is often categorized as a combination of wind, cold, and dampness, together with heat-dampness and phlegm stagnation, all of which culminate in obstructed meridians and poor circulation of qi and blood. [3–4] The disease was first recorded in the “Huangdi Neijing (Yellow Emperor’s Inner Canon),” where systematic documentation of its cause, pathogenesis, symptoms and other related conditions were recorded. According to TCM principles, KOA stems from internal Zheng-qi deficiency, which allows external pathogens or injuries to damage meridians, leading to stagnant blood and consequent pathological responses. [5] The overall pathogenesis of KOA is often attributed to kidney and liver blood deficiency, external injuries, or external invasion of wind, cold, and dampness. [6]
Renowned Chinese TCM physician, Professor Jin Rui, uses a protocolized group of acupoints for treating KOA, named Xisanzhen (three on the knee): Xuehai (SP10), Liangqiu (ST34), Xiyan. Xisanzhen’s main clinical indications are knee pain, swelling, or weakness. Xuehai and Liangqiu regulate blood and qi flow, while Neixiyan and Waixiyan are special acupoints that reduce redness and swelling of the knee. [7]
In important type of acupuncture for KOA is warm needle acupuncture. Warm acupuncture is especially helpful for the treatment of KOA with cold-dampness origin. This type of acupuncture warms the meridians, dispels cold, removes wind and dampness, circulates blood and qi for the purposes of relieving swelling and pain. Fire acupuncture has a similar therapeutic effect.
Centro-square needling, a method of acupuncture wherein extra needles are inserted surrounding the main acupoint, is useful for treating cold-type arthritis. The increased stimulation from the extra needles strengthens the clearing, warming and qi stimulating properties of acupuncture. Centro-square needling is commonly utilized for the treatment of musculoskeletal diseases. [8–10] Centro-square needling to appropriate depths stimulates blood and lymph circulation, promotes the absorption of inflammatory exudates, and calms muscle spasms, thereby aiding tissue regeneration and pain relief. [11]
Zhengzhou Orthopedic Hospital of Traditional Chinese Medicine
A study by Li Jian (Zhengzhou Orthopedic Hospital of Traditional Chinese Medicine) determined that acupuncture enhances patient outcomes for patients taking celecoxib, a non-steroidal anti-inflammatory medication. [12] The study compared KOA patients receiving both acupuncture and celecoxib with KOA patients receiving only celecoxib. Acupuncture provided more significant and longer-lasting pain relief.
To evaluate treatment efficacy, patients were scored based on a KOA grading system and a Visual Analog Scale (VAS). The KOA grading system allocated a total score based on the severity of KOA symptoms. The VAS measures pain intensity levels. KOA and VAS scores were taken thrice throughout the course of the study, once before treatment, once immediately after treatment, and once 8 weeks after treatment. The differences in KOA and VAS scores before and after treatment were recorded.
Results
The improvement in KOA scores for the acupuncture plus drug group was 13.9 ± 2.86 immediately after treatment, while that of the drug group was significantly less (P<0.05) at 12.1 ± 3.51. Eight weeks after treatment, the acupuncture plus drug group maintained a significant improvement of 12.7 ± 2.99, while the drug only group declined (P<0.05) and only achieved a final improvement of 6.51 ± 2.66.
The VAS scores showed a similar trend. Immediately after treatment, the acupuncture plus drug group recorded a VAS improvement of 5.78 ± 0.98, significantly higher than that of the drug group, which was 4.59 ± 1.45 (P<0.05). Eight weeks after treatment, the final VAS improvement of the acupuncture plus drug group was 5.09 ± 0.95, while that of the drug only group fell to 2.40 ± 1.01 (P<0.05). The researchers conclude that acupuncture significantly boost treatment efficacy for patients taking the NSAID celecoxib.
Design
The study was set up as a two-arm experiment. A total of 70 liver and kidney deficient KOA patients from Zhengzhou Orthopedic Hospital of Traditional Chinese Medicine participated in the study. They were diagnosed between March 2014 and October 2016. KOA diagnoses were made based on both TCM and biomedical diagnostic criteria. TCM differential diagnostics were used to diagnose liver and kidney deficiencies and biomedical diagnostic criteria were used to diagnose KOA. TCM diagnostic criteria for liver and kidney deficiency and joint-meridian obstruction were in accordance with the 2002 edition of “Guiding Principles for Clinical Study of New Chinese Medicines.” [13] The TCM guidelines included the following:
- Primary symptoms: Joint pain, soreness/weakness in lower limbs.
- Secondary symptoms: Restricted movement, reddish tongue, thin or white tongue coating, slippery or taut pulse.
- Biomedical diagnostic criteria for KOA were in accordance with “Guidebook for Diagnosis and Treatment of Osteoarthritis” stipulated by the Chinese Orthopedic Association in 2007. [14] The criteria were the following:
- Recurring knee joint pain for ≥1 month.
- Osteophyte (bone spur) formation, subchondral sclerosis and/or cyst formation, joint space narrowing detected via standing/weight-bearing imaging.
- ≥2 synovial fluid analyses performed, synovial fluid clear and sticky with white blood cell count of <2000 cells/ml.
- Morning stiffness ≤30 minutes.
- Crepitus upon movement.
The following selection criteria were also applied:
- Fulfilled both aforementioned TCM and biomedical diagnostic criteria.
- Duration of illness between 4 months and 15 years.
- Discontinued usage of non-steroidal anti-inflammatory drugs, steroids, and other relevant drugs ≥90 days before start of study.
- Complied fully with prescribed treatment during study.
The following exclusion criteria were applied:
- Major orthopedic diseases such as torn meniscus, ligament rupture, vascular/nerve damage, bone tuberculosis and bone tumors.
- Severe psychological or cardiac diseases.
- Pregnant or lactating.
Participating patients were randomly divided into the treatment group and the control group. Both groups were comparable demographically. The treatment group had 35 patients, 10 males, 25 females, aged 46–69 years, mean age 53.7 ± 3.9 year, duration of illness 0.6–14 years, mean duration of illness 5.03 ± 2.23 years. The control group had 35 patients, 9 males, 26 females, aged 45–72 years, mean age 54.2 ± 3.8 years, duration of illness 0.7–16 years, mean duration of illness 4.96 ± 1.3 years.
Both groups were treated with celecoxib. In addition, the treatment group received Xisanzhen acupuncture. Treatment lasted for 6 weeks. During the entire course of treatment, patients discontinued any non-prescribed medications other than those for heart, high blood pressure, diabetes, or infectious diseases.
Acupuncture Treatment
The following acupoints were selected for the treatment group (on the afflicted side):
- Xuehai (SP10)
- Liangqiu (ST34)
- Neixiyan
- Waixiyan
Forty millimeter acupuncture needles were used. Acupoints were located with the knees bent. Xuehai and Liangqiu were vertically pierced 25–30 mm deep, until deqi was achieved. Neixiyan and Waixiyan were pierced inwards, to a 25–30 mm depth, avoiding the joint cavity. One acupuncture session was conducted every other day, thrice per week. Celecoxib capsules (Pfizer Inc., 0.2 g x 6 capsules/box) were orally administered to all patients. The prescribed dosage was 0.2 g each time, once per day, every other day. The results indicate that the addition of acupuncture to a protocol of celecoxib significantly enhances treatment outcomes. Acupuncture provides great pain relief and lasting results.
Nujiang Hospital of Traditional Chinese Medicine
Wang Qirun (Nujiang Hospital of Traditional Chinese Medicine) finds that adding warm needle acupuncture to herbal treatment produces superior positive patient outcomes to using only herbal medicine. [15] The study compared two groups of KOA patients, one receiving only TCM herbs and the other receiving both herbs and warm needle acupuncture. The addition of warm needle acupuncture produces greater pain relief, knee mobility, and knee function.
Three parameters were used to evaluate treatment efficacy: knee pain, knee function, and knee mobility. [16] The Numeric Pain Rating Scale (NRS) was used to provide a quantifiable measure of the intensity of knee pain. From a scale of 0–10 (10 represents the most intense pain), patients selected an integer representing their perceived pain. Knee function was measured using the Hospital for Special Surgery (HSS) score. Finally, knee mobility was recorded as the greatest angle that patients could bend their knee (0°–130°). In addition to the above parameters, each treatment was also given an overall treatment effective rate. Based on clinical symptoms, the treatment efficacy for each patient was classified into 1 of 3 tiers:
- Significantly effective: No knee pain and swelling. Significant improvement in knee mobility.
- Effective: Knee pain and swelling subsided. Improvement in knee mobility.
- Ineffective: No improvement in knee pain, swelling or mobility.
Results
The treatment effective rate for each patient group was derived with the following formula: [Significantly effective + Effective] / [Total number of patients in group] * 100%. The treatment effective rate for the acupuncture plus herbs group was 95.45%, significantly higher than that for the herbs only group (P<0.05), which was 80.95%. The outcome rates show that acupuncture generally strengthens the efficacy of TCM herbal treatment for KOA.
Before treatment, the three parameters of quantification did not differ meaningfully between both groups (P>0.05). The mean NRS scores were 6.73 ± 0.85 and 6.63 ± 0.54 for herbs only and acupuncture plus herbs respectively. The respective mean HSS scores were 45.33 ± 6.74 and 45.42 ± 6.83. The respective mean knee mobility angles were 105.33 ± 6.74 and 105.42 ± 6.83. Both groups started out at a statistically comparable level.
After treatment, both groups showed a marked difference across all 3 parameters. The mean NRS score was reduced to 2.47 ± 0.18 after acupuncture with herbs, while standalone herbal therapy also produced pain reduction (P<0.05), with a final mean NRS score of 3.52 ± 0.64. To the same effect, acupuncture with herbs led to a greater improvement in knee function over the use of herbs as a standalone therapy (P<0.05). The mean HSS scores were 78.52 ± 9.33 and 61.85 ± 7.44 for acupuncture plus herbs and herbs only respectively. Patients had greater knee mobility with acupuncture plus herbs therapy compared with herbs only (P<0.05). The mean knee mobility angles were 128.52° ± 9.33° and 111.85° ± 7.44° for acupuncture plus herbs and herbs respectively.
Design
The study was designed as a double-arm experiment. A total of 43 KOA patients from Nujiang Hospital of Traditional Chinese Medicine participated in the study. Patients were randomly divided into two groups: herbs and acupuncture plus herbs. For an unbiased comparison, the study ensured that both groups were equivalent in demographics at the outset of the investigation (P>0.05). The herbs group had 21 patients, 13 males, 8 females, between 34–76 years, mean age 48.14 ± 2.24 years, duration of illness 1–15 years, mean duration of illness 6.29 ± 0.21 years. The acupuncture plus herbs group had 22 patients, 14 males, 8 females, between 34–74 years, mean age 48.34 ± 2.63 years, duration of illness 1–15 years, mean duration of illness 6.24 ± 0.12 years.
Both groups were given a modified Yi Shen Tong Luo Fang decoction. In addition, the acupuncture plus herbs group received warm acupuncture. The following acupoints were applied with warm needle acupuncture:
- Neixiyan
- Waixiyan
- Zusanli (ST36)
- Heding (MLE27)
- Liangqiu (ST34)
- Xuehai (SP10)
- Yinlingquan (SP9)
- Yanglingquan (GB34)
- Sanyinjiao (SP6)
Size 0.3 mm x 40 mm Hwato brand disposable acupuncture needles were used. Acupuncture was administered with patients in a seated position, knees bent at 90°. Needles were perpendicularly inserted then moderately manipulated by rotation, applying reinforcement-attenuation techniques, until deqi was achieved. For Neixiyan, Waixiyan, and Zusanli, a 2 cm moxa cigar cutting was attached to the end of each inserted needle, then lit. A new moxa cigar cutting was affixed once the previous cigar extinguished. A total of 2 moxa cigars were used for each acupoint per session. During warm needle acupuncture, the acupuncturist ensured that the distance between the skin and moxa cigar cutting was 2–3 cm. To avoid burns, the area surrounding the acupoint was covered with cardboard. All needles were retained for 30 minutes. One acupuncture session was administered per day. One treatment cycle comprised 10 consecutive days of acupuncture, with a 3-day break before the next cycle. [17] Treatment was administered for 2 treatment cycles. The Yi Shen Tong Luo Fang decoction consisted of the following ingredients:
- Tusizi (20g)
- Niuxi (20g)
- Nuzhenzi (15g)
- Gouqizi (15g)
- Buguzhi (15g)
- Chuanxiong (15g)
- Danggui (15g)
- Roucongrong (10g)
- Yinyanghuo (10g)
- Taoren (10g)
- Honghua (10g)
- Zelan (10g)
- Lujiaojiao (10g)
- Paoshanjia (6g)
- Xixin (3g)
- Shenggancao (6g)
Secondary ingredients were added based on TCM differential diagnostics on an individual basis. For phlegm stagnation, the following herbs were added:
- Cangzhu
- Banxia
- Chenpi
For qi-blood deficiency, the following herbs were added:
- Huangqi
- Fuling
For liver-kidney deficiency, the following herbs were added:
- Duzhong
- Xuduan
- Guiban
For wind-cold-dampness obstruction, the following herbs were added:
- Jianghuang
- Rougui
- Fuzi
For wind-damp-heat stagnation, the following herbs were added:
- Huangbai
- Rendongteng
- Xuanshen
One brewing of the decoction was ingested per day. Each brew was divided into two equal portions, one taken in the morning and the other at night. One treatment cycle comprised 10 consecutive days of consumption, with a 3 day break before the next treatment cycle.
Acupuncture plus herbs produced an NRS score of 2.47 ± 0.18 and standalone herbal therapy produced a final NRS score of 3.52 ± 0.64. This demonstrates that adding acupuncture to the herbal medicine protocol enhances the analgesic effects of treatment. Knee function also improved, with a mean HSS score of 78.52 ± 9.33 and 61.85 ± 7.44 for acupuncture plus herbs and herbs only respectively. Mean knee mobility angle improvements were 128.52° ± 9.33° and 111.85° ± 7.44° for acupuncture plus herbs and herbs only respectively. The results indicate that acupuncture plus herbs produces significant positive patient outcomes for patients with knee osteoarthritis.
China Academy of Chinese Medical Sciences
Wang et al. (China Academy of Chinese Medical Sciences) compared the efficacy of two types of acupuncture. [18] Fire acupuncture with centro-square needling and standard acupuncture both produced significant results for patients with KOA, with centro-square needling producing slightly better outcomes.
Pain intensity and osteoarthritis severity were assessed to evaluate clinical efficacy. A VAS was used to measure pain intensity. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) were used to provide a quantifiable measure of KOA severity. [19] Patients were scored on five aspects: pain, joint stiffness, joint physiological function, socialization, and mood. The higher the score, the greater the KOA severity. Based on the WOMAC scores, the improvement rate for each patient was calculated using the following formula: [Score before treatment–Score after treatment] / [Score before treatment] * 100%. The WOMAC improvement rates were then used to categorize the treatment efficacy for each patient into 1 of 4 tiers:
- Clinical recovery: Symptoms completely absent. Normal mobility. WOMAC improvement rate ≥ 95%.
- Significantly effective: Symptoms largely absent. Joint mobility not restricted. WOMAC improvement rate ≥70% but <95%.
- Effective: Symptoms mostly absent, albeit occasional recurrence. Joint mobility slightly restricted. WOMAC improvement rate ≥30% but <70%.
- Ineffective: No noticeable improvement in symptoms and mobility. WOMAC improvement rate <30%.
Based on the number of patients in each tier, the treatment total effective rate for each patient group was calculated using the following formula: [Clinical recovery + Significantly effective + Effective] / [Total number of patients in group] * 100%. The treatment significantly effective rate was calculated using the following formula: [Clinical recovery + Significantly effective] / [Total number of patients in group] * 100%. Patient evaluations were conducted four times: before treatment, 2 weeks into treatment, 4 weeks into treatment, and 1 month after treatment.
Results
The VAS scores showed significant improvement in both groups after treatment. For the fire centro-square acupuncture group, the VAS score was 6.94 ± 1.64 before treatment, with a steady reduction throughout treatment. The VAS scores were 3.88 ± 1.25 two weeks into treatment, 2.29 ± 1.13 four weeks into treatment, and 1.73 ± 1.11 one month after treatment. Similarly, for the filiform acupuncture group, the VAS score was 6.89 ± 1.83 before treatment, 4.83 ± 1.91 two weeks into treatment, 3.09 ± 1.82 four weeks into treatment, and 2.55 ± 1.55 one month after treatment.
Both groups saw consistent improvement throughout the course of treatment for all datapoints. The VAS scores one month after treatment also illustrate that the therapeutic effect of acupuncture for KOA lasts beyond the treatment time-frame, showing that patients experience pain relief even after they discontinue treatment. At the same time, the fire centro-square acupuncture group achieved greater improvements than the filiform acupuncture group at all three datapoints after treatment.
The WOMAC scores display a similar trend. For the fire centro-square acupuncture group, the WOMAC scores were 89.97 ± 23.04 before treatment, 52.83 ± 20.85 two weeks into treatment, 29.44 ± 16.81 four weeks into treatment, and 22.03 ± 17.21 one month after treatment. This demonstrates that KOA symptoms were consistently lessening throughout the treatment period and continued to improve even after treatment ended (P < 0.01). The filiform acupuncture group also showed a stable decline in WOMAC scores (P < 0.01). The scores were 88.53 ± 26.77 before treatment, 59.92 ± 23.80 two weeks into treatment, 39.83 ± 23.46 four weeks into treatment, and 31.83 ± 21.16 one month after treatment. From 4 weeks into treatment onwards, the fire centro-square acupuncture group achieved lower WOMAC scores than the filiform acupuncture group (P<0.05). Both groups achieved significant positive patient outcomes.
The treatment effective rates are reflective of the VAS and WOMAC results. Two weeks into treatment, the fire centro-square acupuncture group had a 2.8% significantly effective rate, and an 88.9% total effective rate. The filiform acupuncture group had a slower initial improvement (P<0.01), having a 0% significantly effective rate and a 61.1% total effective rate. Further along into the treatment at 4 weeks, the significantly effective rate of the fire centro-square acupuncture group increased to 66.7%, bringing the total effective rate to 97.2%, while the filiform acupuncture group had a 41.7% significantly effective rate and a 91.7% total effective rate. At 4 weeks into treatment, more patients saw significant efficacy with fire centro-square acupuncture than conventional filiform acupuncture (P<0.05). One month after treatment ended, the data reflects that patient symptoms continue to improve. The significantly effective rate of the fire centro-square acupuncture group was 83.3%, and the total effective rate remained at 97.2%. This was greater than the conventional filiform acupuncture group (P<0.01), which had a significantly effective rate of 44.4% and total effective rate of 94.4%.
Design
The study was designed as a double-arm experiment. A total of 72 KOA patients from the Acupuncture and Moxibustion Hospital (Institute of Acupuncture and Moxibustion of China Academy of Chinese Medical Sciences) participated in the study. Patients were divided into either the fire centro-square group or the conventional filiform acupuncture group, with 36 patients in each group. Both groups were equivalent (P>0.05) in gender, age, and duration of illness prior to the investigation to ensure a fair comparison.
The fire centro-square group had 16 males, 20 females, aged between 40–75 years, mean age 59 ± 9 years, duration of illness between 0.8–240 months, mean duration of illness 39.8 ± 53.1 months. The filiform group had 9 males, 27 females, aged between 40–75 years, mean age 56 ± 11 years, duration of illness between 1.0–240 months, mean duration of illness 42.8 ± 53.4 months. All 72 patients were included in the final results and no subjects were disqualified for non-compliance with treatment or severe side effects during the study.
The diagnostic criteria for KOA were in accordance with those published by the American College of Rheumatology, which were recommended in the “Osteoarthritis Diagnosis and Treatment Guide” drafted by the Rheumatology Committee of the Chinese Medical Association. [20] These criteria were the following:
- Frequent knee joint pain (most of the time) within the recent month.
- Presence of crepitus.
- Knee joint morning stiffness lasting ≤30 minutes.
- ≥40 years old.
- Swelling around knee joint.
- Bone spurs around the bone edges of the knee, detected by X-ray.
The diagnosis was confirmed if the patient fulfilled both conditions 1 and 6, or conditions 1 through 5. The following selection criteria were applied to choose trial participants:
- Fulfilled the diagnostic criteria.
- Did not receive any KOA treatment, or other treatments that may affect the study results, within the recent month.
- VAS score of ≥3.
- Signed informed consent.
The following exclusion criteria were applied:
- Knee synovitis, meniscus injury or cruciate ligament injury.
- Rheumatoid arthritis, metabolic arthritis or other non-osteoarthritic diseases that may cause knee pain.
- History of knee surgery or severe knee injury.
- Other diseases with complications affecting the joints, such as psoriasis, syphilitic neuropathy, ochronosis, metabolic bone diseases, acute trauma etc.
- Severe cardiac, neurological, hepatic, renal, respiratory, hematopoietic or mental diseases.
- Prone to spontaneous bleeding.
- Pregnant or lactating.
Acupoint selection was identical for both groups. Three acupuncture sessions were administered per week. Sessions were administered one day apart from another, with Sunday being a break day. One treatment cycle was comprised of six acupuncture sessions, and a total of two treatment cycles were administered. The following primary acupoints were selected and applied to the afflicted side):
- Xuehai (SP10)
- Liangqiu (ST34)
- Neixiyan
- Dubi (ST35)
- Zusanli (ST36)
- Yanglingquan (GB34)
- Yinlingquan (SP9)
- Ashi
The patients rested in a supine position during acupuncture. Size 40 mm length needles were used on most acupoints. The following protocol was observed for the fire centro-square group. Needles were heated using an ethanol lamp untill the tip and body were red-hot, then perpendicularly inserted into each acupoint in a swift motion, to 20–30 mm depth, and retained for 3–5 minutes. For Neixiyan and Dubi, 25 mm length needles were used instead, inserted swiftly 5 mm deep and not retained. Centro-square needling was carried out on the Ashi acupoints. Additional needles were inserted around each Ashi acupoint, at 4 centro-square points, each deviating 1–1.5 inches away from the Ashi acupoint: above, below, left and right.
At each centro-square point, a heated needle was inserted at a 30–40° angle toward the Ashi acupoint, to 20–30 mm depth, then retained for 3–5 minutes. If an Ashi acupoint was located near the edge of the kneecap or either end of the knee joint where the flesh was thin, a 25 mm long needle was used, and the depth of insertion was adjusted to 10–20 mm. Apart from the Ashi acupoints, two of the other selected acupoints (barring Neixiyan and Dubi) were targeted for centro-square needling in one acupuncture session, and a different pair was targeted in every session. After needle removal, the pierced acupoints were immediately cupped, retaining the cups for 3–5 minutes. The following measures were observed during treatment:
- After fire acupuncture, the treated areas were disinfected with iodine.
- Patients were advised to avoid showering on the day of acupuncture, and to keep the treated areas dry.
- Patients were instructed to refrain from scratching the treated areas after acupuncture, as slight reddening, itching, or swelling are normal reactions.
The following protocol was observed for the filiform group. Conventional filiform needle acupuncture was administered after disinfection. Upon achieving deqi, the needles were manipulated with reinforcement and attenuation (Ping Bu Ping Xie), then retained for 30 minutes. Ashi acupoints, as well as two of the other treated acupoints, were immediately cupped after needle removal. A different pair of acupoints were cupped in each session. Both types of acupuncture achieved significant positive patient outcomes.
Summary
Knee osteoarthritis is often a painful and disabling disorder. Research confirms that acupuncture is an effective treatment modality for short and long-term relief. Patients with knee osteoarthritis are advised to consult with local licensed acupuncturists to learn more.
References
1. Le ZQ, Tao P, Le SS, et al. Clinical efficacy observation of warm acupuncture combined with Yishentongluofang brew in treating KOA [J]. Guangming Journal of Chinese Medicine, 2016, 31(5): 618-620.
2. Huang Y. Clinical efficacy observation of warm acupuncture combined with TCM herbs differential treatment of KOA [J]. Inner Mongol Journal of Traditional Chinese Medicine, 2015, 34(1): 66-67.
3. Yu QY, Huang W. Discussion of pathogenesis and symptoms of KOA from the perspective of “Bi” [J]. Rheumatism and Arthritis, 2015, 4(3): 40-43.
4. Zhang L, Wang YP, Yin YS, et al. Musculoskeletal ultrasound observation of soft tissue changes after needle-knife acupuncture in treating KOA [J]. China Journal of Orthopedics and Traumatology, 2014, 27(1): 17-20.
5. Li C, Jiang B, Jin J. Progress of research on TCM medicine in treating KOA [J]. Hunan Journal of Traditional Chinese Medicine, 2013, 29(1): 136-137.
6. Tang XP, Hu Y, Wang F. Experience of Professor Hu Yinqi in diagnosing rheumatoid arthritis [J]. Journal of Basic Chinese Medicine, 2013, 19(2): 220-222.
7. Zhang HY. Clinical research on TCM herbs combined with acupuncture in treating KOA [D]. Jinan: Shandong University of Traditional Chinese Medicine, 2013.
8. Li XH, Li DJ. Efficacy observation of using mainly centro-square needling of Dazhui acupoint in treating cervical spondylosis [J]. Chinese Acupuncture & Moxibustion, 2004, 24(7): 13-14.
9. Zhong MY, Wu SP. Clinical observation of centro-square needling of movement pain points combined with function training in treating adhesive capsulitis [J]. Journal of Traditional Chinese Medicine University of Hunan, 2015, 35(3): 60-63.
10. Yao CY. 128 cases of treating rheumatic arthritis with mainly centro-square needling [J]. Journal of Practical Traditional Chinese Internal Medicine, 2005, 19(5): 483.
11. Gao YX, Liu XX. 46 cases of treating lumbar disc herniation with centro-square acupoint injection combined with iontophoresis [J]. Shandong Journal of Traditional Chinese Medicine, 2007, 26(1): 37-38.
12. Li J. Clinical Observation on Knee Tri-Acupuncture in the Treatment of Knee Osteoarthritis for 35 Cases [J]. Guangming Journal of Chinese Medicine, 2017, 32(10): 1458-1460.
13. Zheng XY. Guiding Principles for Clinical Study of New Chinese Medicines [M]. Beijing: China Medical Science Press, 2002: 349.
14. Chinese Orthopedic Association. Guidebook for Diagnosis and Treatment of Osteoarthritis (2007 edition) [J]. Chinese Journal of Clinical Medicine, 2008, 36(1): 28-30.
15. Wang QR. Clinical research on warm acupuncture combined with Yishentongluofang brew in treating KOA [J]. Asia-Pacific Traditional Medicine, 2017, 13(20): 137-138.
16. Li CQ. Warm acupuncture combined with TCM herbs differential treatment of KOA 80 cases [J]. Journal of Community Medicine: Professional Medicine, 2010, 12(26): 125.
17. Lan SX. Efficacy observation of warm acupuncture combined with TCM herbs differential treatment of KOA [J]. Inner Mongol Journal of Traditional Chinese Medicine, 2013, 32(30): 80-81.
18. Wang B, Hu J, Zhang N, et al. Clinical study of fire acupuncture with centro-square needles for knee osteoarthritis [J]. Chinese Acupuncture & Moxibustion, 2017, 37(5): 463-476.
19. Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee [J]. Rheumatol, 1988, 15(2): 1833–1840.
20. Rheumatology Committee of the Chinese Medical Association. Osteoarthritis Diagnosis and Treatment Guide (Draft) [J]. Chinese Journal of Rheumatology, 2003, 7(11): 702-704.
From HealthCMi news articles.
